Author: Laura Cowen
medwireNews: The incidence of thrombosis among people receiving the CDK4/6 inhibitor abemaciclib for metastatic breast cancer is approximately threefold higher in a real-world setting than that observed in clinical trials, US study data show.
“Given these findings, studies evaluating the role of thromboprophylaxis in patients receiving abemaciclib are needed,” write Hanny Al-Samkari (Massachusetts General Hospital, Boston) and co-authors in Cancer.
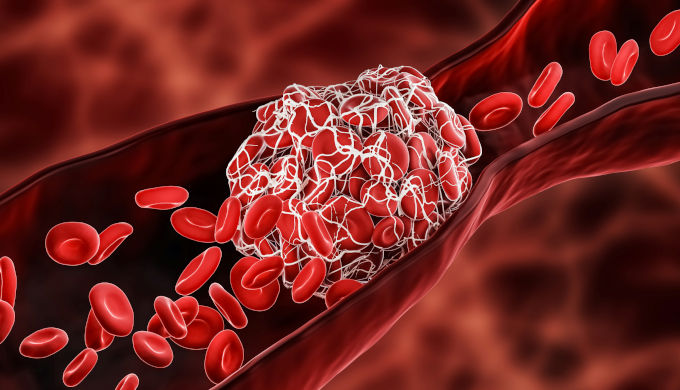
They explain that abemaciclib already has a black-box warning for increased venous thromboembolism (VTE) risk on its FDA label as a result of clinical trial data, but thrombosis rates in real-world populations are unclear.
The researchers therefore reviewed data for 364 patients with metastatic breast cancer who received abemaciclib at five hospitals between 2017 and 2021.
During a median 5.5 months of therapy, 26 patients developed 27 thrombotic events, giving an event rate of 7.4%. These included VTE in 4.7% and arterial thrombosis in 2.5%. One (0.3%) patient experienced both events.
Pulmonary embolism (PE) was the most common VTE event, occurring in seven (1.9%) patients. Three (0.8%) additional patients had PE with a concurrent deep vein thrombosis. Stroke was the most common arterial thrombotic event, with four (1.1%) patients affected.
When the investigators compared their data with findings from the MONARCH 2 and 3 trials, which provided evidence for FDA approval of abemaciclib as well as the black-box warning, they found that the incidence of thrombosis was two to three times higher in the real-world setting.
Specifically, total thrombosis occurred at a rate of 13.7 events per 100 person–years in this cohort compared with rates of 4.1 and 4.9 events per 100 person–years in the MONARCH 2 and 3 trials, respectively.
The rate of VTE was 9.1 events per 100 person–years in the current cohort versus 4.1 and 4.9 events per 100 person–years in MONARCH 2 and 3, respectively. Of note, there were no cases of arterial thrombosis in the two clinical trials.
Al-Samkari and team note that 18.4% of patients in the current study had a history of VTE and 5.8% had a history of arterial thrombosis, while 44.5% and 35.7% had hypertension and hyperlipidemia, respectively. Despite the presence of these risk factors multivariable analyses did show any significant associations between baseline characteristics and VTE risk.
There was, however, a significant 2.1-fold increased risk for death among the people who developed VTE during therapy relative to those who did not, with median overall survival at 9.6 and 25.8 months in the former and latter groups, respectively.
Al-Samkari et al conclude that their study confirms that the black-box labeling “is not only warranted, but that the thrombotic rates in real-world populations appear to be even higher” than those in clinical trials.
They add: “Our findings are particularly important because abemaciclib has recently become the first and only CDK 4/6 inhibitor to date to be approved for use beyond the metastatic disease setting.”
medwireNews is an independent medical news service provided by Springer Healthcare Ltd. © 2022 Springer Healthcare Ltd, part of the Springer Nature Group
Image Credits: © ibre de droit / Getty Images / iStock